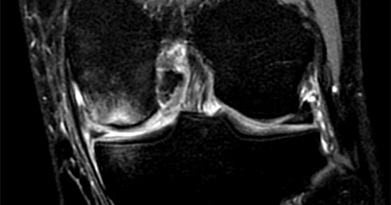
Figure 1
Subchondral fractures are injuries that occur in the knee most commonly in the setting of acute injuries. They can also occur in patients with preexisting degenerative changes in the knee.
Subchondral bone fractures can happen when the load on the joint is transmitted beyond the protective measures of the menisci, which are shock absorbers, and the articular cartilage. Seemingly minor injuries which results in meniscal injuries increase femoral tibial axial contact pressures. These alter the normal knee biomechanics, which can cause a subchondral knee fracture (Figure 1). In addition subchondral fractures, sometimes referred to as bone bruises, can also occur from direct impact to the knee during activity.
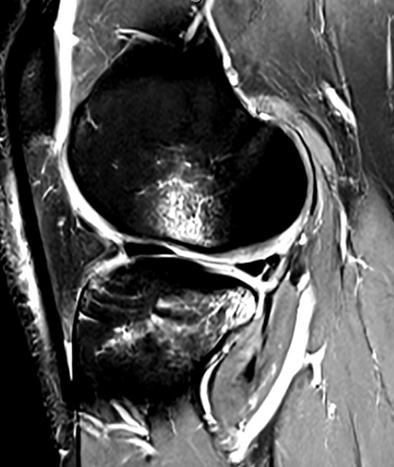
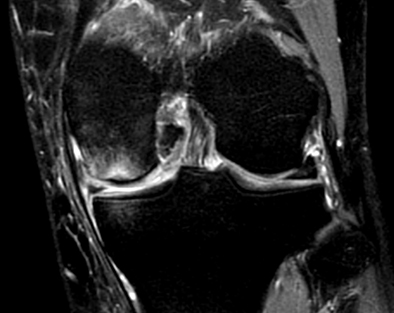
Figure 2
Subchondral knee fractures of the knee are also common occurrences with ligament injuries such as ACL tears. Oftentimes, with the pivot shift mechanism in an ACL rupture there is an anterior translation of the tibia relative to the femur. When this happens, there is frequently bone bruising also called subchondral fractures noted in the posterior lateral tibial plateau and anterior lateral femoral condyles. MRIs will show these lesions in the acute period. This is often referred to as kissing contusions (Figure 2).
Subchondral knee fractures are also common in older patients with osteoporotic bone. If the subchondral fracture is bad enough, it can often progress to osteonecrosis and collapse of the subchondral bone. The goal of the treatment of subchondral knee fractures is to prevent the progression of osteoarthritis which may ultimately need a total knee replacement. Conservative management is the first choice of treating early stages of subchondral knee fractures. This includes protected weight bearing and non-steroidal anti inflammatory medications. It usually takes several months for a subchondral fracture to heal with conservative management. If conservative management fails, surgical treatment is an option and can involve providing support to the subchondral area through screw fixation or a subchondroplasty/bioplasty procedure.
This blog post is for educational purposes only. Please consult with a board-certified orthopedic surgeon when seeking treatment for musculoskeletal care.